Abstract
Introduction: Vasoactive intestinal peptide (VIP) is an anti-inflammatory neuropeptide known to induce differentiation of regulatory dendritic cells and regulatory T cells. Using allogeneic hematopoietic stem cell transplantation (allo-HSCT) models, we have shown that donor bone marrow (BM) plasmacytoid dendritic cells (pDCs) facilitate HSC engraftment and attenuate pathogenesis of graft vs. host disease (GvHD) through regulation of recipient T cells. However, the mechanism by which pDCs mitigate the GvHD activity of recipient T cells is not clearly understood. Here, we report that donor pDCs limit pathogenic T cell inflammation by VIP production.
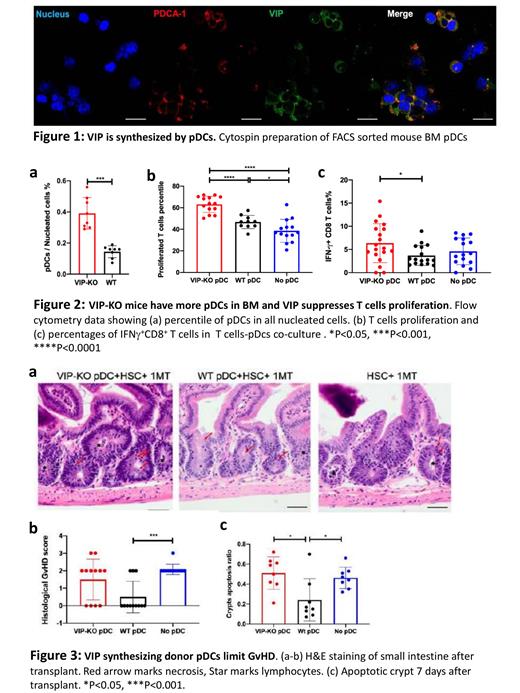
Methods: To study VIP production by pDCs, FACS-sorted pDCs from B6 mouse BM were cultured with or without PMA/ionomycin in-vitro. After activation and cytospin slide preparation, pDCs were labeled with anti-PDCA1 (pDC marker) and anti-VIP antibodies for confocal fluorescence microscopy. To investigate the effects of VIP production on T cell proliferation, an in-vitro co-culture assay was performed using R848 and CpG-activated WT or VIP-KO pDCs with anti-CD3-activated, CFSE-labeled syngeneic T cells. For GvHD experiments, irradiated B10.BR (H-2K k) mice received 5x10 3 HSCs, 5x10 4 pDCs and 1x10 6 T cells from WT B6 (H-2K b) or VIP-KO B6 (H-2K b) mice. H&E histology of intestine and colon was performed for GvHD scoring 7 days post-transplant. Graft vs. leukemia (GvL) effects were tested by inoculating recipient mice with 5x10 5 LBRM 33-5A4 cells in the same model. Recipient mice were monitored twice weekly using a 10-point GvHD scoring system. Gene expression analysis of FACS-sorted donor T-cells from recipient spleens was performed using the Nanostring Myeloid Innate Immunity Panel at days 8 and 15 post-transplant.
Results: Confocal microscopic images of PMA/ionomycin stimulated or unstimulated sorted pDCs show that VIP is synthesized by pDCs (anti-VIP, green; anti-PCDA-1, red; DAPI counterstain, blue) (Fig 1). After in-vitro culture, VIP expression and frequencies of VIP + pDCs were similar in PMA/ionomycin treated or untreated cells (not shown). VIP-KO mice have significantly higher percentages of pDCs in BM compared to WT (Fig 2a). T cells co-cultured with VIP-KO pDCs showed higher proliferation than T cells co-cultured with WT pDCs, demonstrating that VIP secreted by pDCs reduces T cell proliferation (Fig 2b). Moreover, VIP-KO pDCs induce significantly greater proliferation of IFN-gamma + CD8 T cells compared to WT, indicating that pDCs lacking VIP promote Th1 polarization in-vitro (Fig 2c). The data are consistent with results from GvHD experiments showing increased frequencies of Th1 polarized T cells and fewer regulatory T cells in recipients of VIP-KO pDCs compared with recipients of WT pDCs. Intestinal GvHD scores and crypt apoptosis in the colon were higher in recipient groups transplanted without pDCs or with VIP-KO pDCs compared with recipients of WT pDCs (Fig 3a, b, c). These results indicate that VIP secreted from pDCs limits GvHD in the gut. In the GvL model, administration of pDCs lacking VIP did not alter the anti-tumor effect of donor T cells. Nanostring analysis of T cells recovered from VIP-KO pDC recipients had increased expression of the pro-inflammatory transcription factor Bhlhe40 during the first two weeks post-transplant, and higher transcription levels of the inflammatory mediator Cyclophilin A at day 15 post-transplant than T cells from recipients of WT pDCs.
Conclusion: Data from in vitro and in vivo experiments suggest that VIP secreted by pDCs limits pathogenic T cell proliferation. In murine allo-BMT, increased gut GvHD scores and crypt apoptosis in recipients transplanted without pDCs or with VIP-KO pDCs indicates that VIP secreted by pDCs consolidates gut integrity without altering GvL. Gene expression analysis also supports a mechanism by which VIP-secreting donor pDCs reduce T cell inflammation through negative regulation of Bhlhe40. Our findings suggest paracrine VIP signaling is a novel immune checkpoint pathway by which donor pDCs limit T cell activation, Th1 polarization, and inflammation, and improve outcomes of allo-BMT by reducing GvHD activity.
Waller: Cambium Oncology: Current holder of individual stocks in a privately-held company, Current holder of stock options in a privately-held company; Verastem Oncology: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal